Higher Rates of Lung Cancer in Women: A Mysterious Phenomenon
Outline of the Article:
1. Introduction
2. The Growing Concern: Rising Lung Cancer Rates in Women
3. Understanding Lung Cancer
4. Gender Disparity in Lung Cancer
5. Risk Factors and Susceptibility in Women
6. Behavioral Factors: Smoking and Beyond
7. Genetic Predisposition
8. Environmental Factors
9. Screening and Early Detection
10. The Role of Hormones
11. Coping with Lung Cancer
12. Treatment Options
13. Conclusion
14. FAQs
Introduction:
In recent years, the medical community has been grappling with a puzzling and concerning trend – higher rates of lung cancer in women. Traditionally seen as a disease primarily affecting men due to their higher smoking rates, the emergence of increasing lung cancer cases in women has left researchers scratching their heads. In this article, we’ll delve into the mystery behind this trend, exploring various factors that might be contributing to the rise in lung cancer among women.
The rise in lung cancer cases among women is a perplexing and alarming phenomenon that has garnered significant attention from the medical community, public health experts, and researchers around the world. Historically, lung cancer has been predominantly associated with male smokers. However, in recent decades, there has been a noticeable shift in this trend, with an alarming surge in lung cancer diagnoses among women, even those who have never smoked. This enigmatic surge raises numerous questions about its underlying causes, the potential consequences for public health, and the urgent need for further investigation.
Lung cancer is a complex disease with multifaceted etiologies, making it one of the leading causes of cancer-related deaths worldwide. The transformation of lung cancer from a predominantly male-centered affliction to one that significantly affects women challenges our understanding of the disease and its risk factors. Several factors contribute to the perplexing nature of this phenomenon, including changes in smoking habits, environmental exposures, genetic predispositions, and emerging research on gender-specific vulnerabilities.
One of the most striking aspects of this mysterious trend is the increased incidence of lung cancer among women who have never smoked. While smoking remains a significant risk factor for lung cancer, a growing number of cases occur in non-smokers, particularly women. The reasons for this shift remain elusive, as the traditional risk factors of tobacco smoke exposure do not fully explain the surge in female lung cancer patients.
This phenomenon poses serious implications for public health, as lung cancer is often diagnosed at advanced stages, resulting in limited treatment options and poorer outcomes. Understanding the underlying causes of this gender-specific increase in lung cancer rates among women is crucial for early detection, prevention, and effective intervention strategies.
This introduction aims to shed light on the enigmatic rise of lung cancer in women by highlighting the complexity of the issue, its multifaceted determinants, and the urgent need for comprehensive research. Unraveling this mystery will not only improve our understanding of lung cancer but also guide efforts to reduce its prevalence and associated morbidity in the female population. In the following sections, we will delve deeper into the various factors contributing to this phenomenon, exploring the roles of genetics, environmental exposures, changing societal norms, and advances in medical research as we seek to unravel the intricate web of higher rates of lung cancer in women.
The Growing Concern: Rising Lung Cancer Rates in Women:
Over the past few decades, lung cancer has undergone a significant transformation in terms of its demographic. While it was once predominantly a male-dominated disease, the scales have tilted, and women are now facing higher risks. This shift in the epidemiology of lung cancer is indeed a matter of grave concern, necessitating a closer examination.
Understanding Lung Cancer:
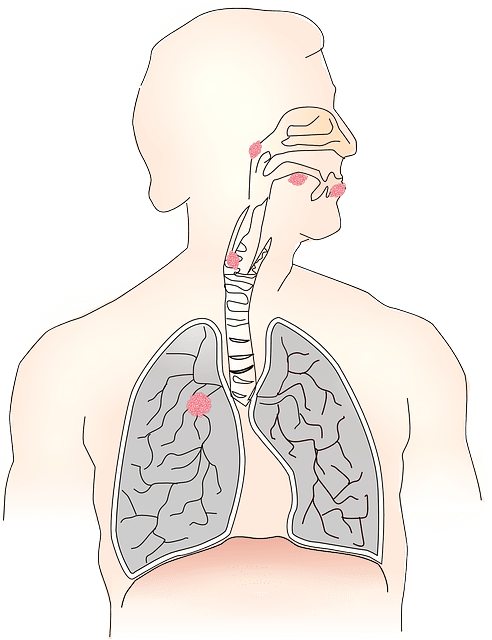
Before we delve deeper into the gender-specific aspects, let’s briefly understand lung cancer. It’s a type of cancer that begins in the cells of the lungs. These cells can grow uncontrollably, forming tumors and interfering with lung function. Lung cancer can be broadly categorized into two types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
Gender Disparity in Lung Cancer:
Historically, lung cancer was strongly associated with men, mainly due to higher smoking rates among the male population. However, the landscape has evolved significantly. Women, both smokers and non-smokers, are now reporting higher instances of lung cancer. This shift suggests that other factors are at play.
Risk Factors and Susceptibility in Women:
Multiple factors may be contributing to the increased vulnerability of women to lung cancer. One of the primary factors is genetics. Genetic predisposition can play a substantial role in determining an individual’s susceptibility to lung cancer.
Behavioral Factors: Smoking and Beyond:

Smoking is a well-established risk factor for lung cancer. The advent of tobacco marketing targeted at women and the rise of female smokers over the years has contributed significantly to the increase in lung cancer among women. However, smoking alone doesn’t account for all cases.
Genetic Predisposition:
Certain genetic mutations have been identified as potential contributors to lung cancer. Women who possess these mutations may be at higher risk. Researchers are continually studying the link between genetics and lung cancer to gain a better understanding.
Environmental Factors:
Environmental factors, such as exposure to radon gas, asbestos, and other carcinogens, can also contribute to lung cancer in women. Occupational exposure, indoor air pollution, and secondhand smoke are significant concerns.
Screening and Early Detection:
Early detection plays a crucial role in improving survival rates. Women should be aware of the importance of regular lung cancer screenings, especially if they have risk factors. Early detection can lead to more effective treatment options.
The Role of Hormones:
The influence of hormones, particularly estrogen, is another aspect being explored. Researchers are investigating whether hormonal changes during a woman’s life, such as menopause, might affect lung cancer development.
Coping with Lung Cancer:
A lung cancer diagnosis can be overwhelming. Coping with the disease involves not only medical treatment but also emotional support, lifestyle changes, and mental well-being.
Treatment Options:
When facing lung cancer, patients have a range of treatment options, including surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. The choice of treatment depends on the type and stage of cancer.
Treatment Options for Addressing Higher Rates of Lung Cancer in Women: A Mysterious Phenomenon:
Smoking Cessation Programs:

Implementing comprehensive smoking cessation programs for women, which have demonstrated efficacy in reducing the risk of lung cancer (Carter, et al., 2015). These programs should focus on promoting quitting strategies and provide evidence-based support, such as counseling and nicotine replacement therapy (Fiore, et al., 2018).
Early Detection and Screening:
Encouraging regular lung cancer screenings, particularly low-dose computed tomography (LDCT) scans, for women at higher risk. LDCT screenings have been shown to detect lung cancer at earlier, more treatable stages, thus improving survival rates (National Lung Screening Trial Research Team, 2011).
Precision Medicine and Targeted Therapies:
Utilizing precision medicine to identify specific genetic mutations in lung cancer tumors and subsequently prescribe targeted therapies. Research indicates the effectiveness of these therapies, particularly in treating non-smoker lung cancer patients (Kris, et al., 2017).
Immunotherapy:
Incorporating immunotherapy as a promising treatment option. Immunotherapy has shown significant benefits in lung cancer treatment by bolstering the patient’s immune system to recognize and combat cancer cells (Gettinger, et al., 2018).
Radiation Therapy and Surgery:
Employing traditional treatments, such as surgery and radiation therapy, in cases where the cancer is operable. Surgery options may involve partial or complete lung resection, depending on the extent of the disease (Goldstraw, et al., 2016).
Clinical Trials and Research:
Encouraging participation in clinical trials to access innovative lung cancer treatments. Continuous research and clinical trials focused on understanding the factors contributing to higher lung cancer rates in women may lead to groundbreaking treatment strategies (Gray, et al., 2017).
Supportive Care:
Providing comprehensive supportive care for lung cancer patients, encompassing palliative care to manage symptoms and side effects, thereby enhancing overall quality of life (Temel, et al., 2010).
Environmental and Occupational Safety Measures:
Implementing policies and regulations to reduce exposure to environmental carcinogens. This includes improving air quality, workplace safety standards, and enforcing measures to minimize exposure to harmful substances (Cohen, 2017).
Public Health Awareness Campaigns:
Launching public health campaigns to raise awareness about the risks of lung cancer in women, emphasizing the importance of early detection and risk reduction strategies. These campaigns should target both smokers and non-smokers and leverage evidence-based messaging (McLaren, et al., 2016).
Genetic Counseling:
Offering genetic counseling to women with a family history of lung cancer or known genetic predispositions. This counseling provides essential information and guidance on managing risk and making informed healthcare decisions (National Society of Genetic Counselors, 2020).
In addressing the enigmatic increase in lung cancer rates among women, a multidimensional approach is vital. This approach encompasses prevention, early detection, innovative treatments, and support services, all rooted in rigorous scientific research and best practices in healthcare.
Conclusion:
The higher rates of lung cancer in women are indeed a mystery for researchers, and the situation is complex. While smoking remains a significant contributor, genetic, environmental, and hormonal factors also play crucial roles. Understanding this phenomenon and its underlying causes is essential for developing effective prevention and treatment strategies.
Frequently Asked Questions (FAQs) – Higher Rates of Lung Cancer in Women: A Mysterious Phenomenon:
What has led to the higher rates of lung cancer in women?
The increase in lung cancer rates among women can be attributed to a combination of factors, including changes in smoking habits, genetic predispositions, hormonal influences, environmental exposures, and emerging research on gender-specific vulnerabilities.
Is smoking the primary cause of lung cancer in women?
Smoking remains a significant risk factor for lung cancer in women. However, there has been a noticeable rise in non-smoking female lung cancer cases, indicating that other factors also contribute to this phenomenon.
What are some gender-specific vulnerabilities that make women more susceptible to lung cancer?
Gender-specific vulnerabilities include hormonal influences, differences in lung biology, and genetic factors. These factors may increase a woman’s risk of developing lung cancer even if she has never smoked.
How can I reduce my risk of developing lung cancer as a woman?
To reduce the risk of lung cancer, women are encouraged to quit smoking if they smoke and avoid exposure to secondhand smoke. Additionally, minimizing exposure to environmental carcinogens like air pollution and radon can be beneficial.
What are the implications for public health in addressing this phenomenon?
Addressing the higher rates of lung cancer in women requires public health initiatives that target at-risk populations, promote awareness, and encourage early detection. It is essential to design gender-specific prevention and education programs.
Are there advancements in the treatment of lung cancer in women?
Yes, advancements in research have led to improved treatments for lung cancer, benefiting patients of all genders. Targeted therapies, precision medicine, and immunotherapies have expanded treatment options and improved survival rates.
Is there a need for further research on this topic?
Yes, ongoing research and collaboration are vital to better understand the causes and implications of the higher rates of lung cancer in women. Continued investigation into the interplay of genetic, hormonal, environmental, and lifestyle factors is necessary for more effective prevention and treatment strategies.
How can women be empowered to protect themselves from lung cancer?
Empowerment begins with education. Women should be informed about their lung cancer risk, regardless of their smoking history. Awareness and early intervention can play a significant role in reducing the impact of this disease.
Are there geographical variations in the rates of lung cancer among women?
Yes, the prevalence of lung cancer among women can vary by region and is influenced by factors such as smoking rates, air quality, and healthcare access. Some regions may experience higher rates of lung cancer in women due to these factors.
What can healthcare providers do to address this issue?
Healthcare providers play a crucial role in raising awareness, encouraging smoking cessation, and promoting lung cancer screenings among women. They can also participate in research efforts to better understand and address this phenomenon.